Table of Contents
Cite this page: Thyroglossal duct cyst. PathologyOutlines.com website. http://www.pathologyoutlines.com/topic/thyroidthyroglossal.html. Accessed October 27th, 2016.
See also
Definition / General
- The most common developmental anomaly of thyroid gland, and the most common congenital neck mass
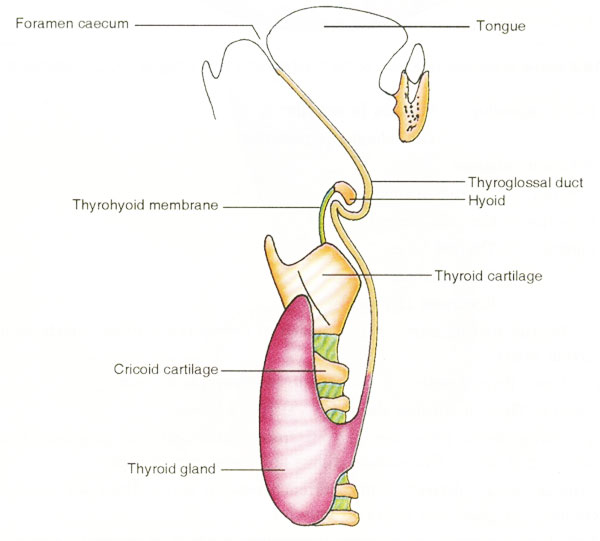
- Midline neck developmental anomaly due to persistence and cystic dilation of thyroglossal duct
- Thyroglossal duct (TGD) is the embryonic tract characterized by the presence of epithelial lined remnants and heterotopic thyroid tissue
- May appear as blind tubular structure in mid neck or as sinus tract connected to foramen cecum or suprasternal notch skin
Terminology
- Synonyms: TGD anomaly, TGD remnant, thyroglossal or thyreoglossal, thyroglossal duct or thyroglossal tract
- Sinus is a blind ending tract lined by granulation tissue leading deep inside from natural / normal epithelial surface, e.g. from cervical skin or foramen cecum to TGD cyst (the latter, even being epithelialized, is not considered as a normal postnatal structure)
- Fistula is a communication between two normal epithelialized surfaces, e.g. between skin and oropharynx via TGD tract / cyst, which is extremely rare (Laryngoscope 2009;119:2345)
- TGD fistula is often used erroneously to represent the discharging sinus
Epidemiology
- TGD cyst is the most common congenital anomaly of the neck in childhood, and the most common developmental neck cyst, accounting for 60 - 70% of all cases (Head Neck Surg 1982;5:134, Auris Nasus Larynx 2008;35:11)
- Mean age 30 - 40 years old, with 65% of cases being diagnosed before 30 years of age, and up to 25% in 50+ year old patients (Am J Surg 1988;155:741)
- Ratio of non-draining cyst to sinus or fistula is 4:1
- Discharging sinuses manifest at younger age (Eur Arch Otorhinolaryngol 2015;272:2513)
- M:F = 1:1 (Head Neck Surg 1982;5:134)
- Serial sections on autopsy identified TGD remnants in 7% of both adult and pediatric cohorts (Laryngoscope 1977;87:765, Ann Otol Rhinol Laryngol 2000;109:1135)
- Scintigraphy after TSH stimulation found TGD remnants in >40% of thyroidectomized patients (Clin Radiol 2015;70:638)
- Out of several thousand TGD cysts described in series and case reports, only 20+ familial cases were published (Pediatr Surg Int 2005;21:593, OMIM - 188455)
Sites
- Appears in midline neck anywhere along path of TGD, from foramen cecum in tongue base to suprasternal region
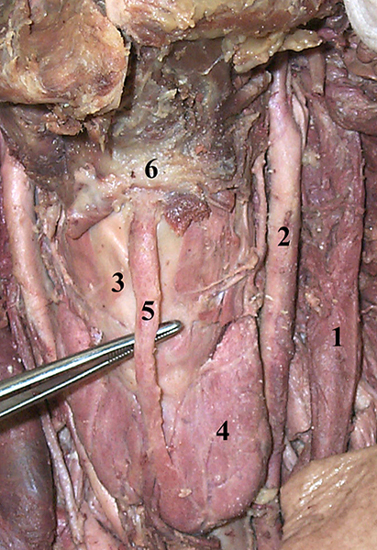
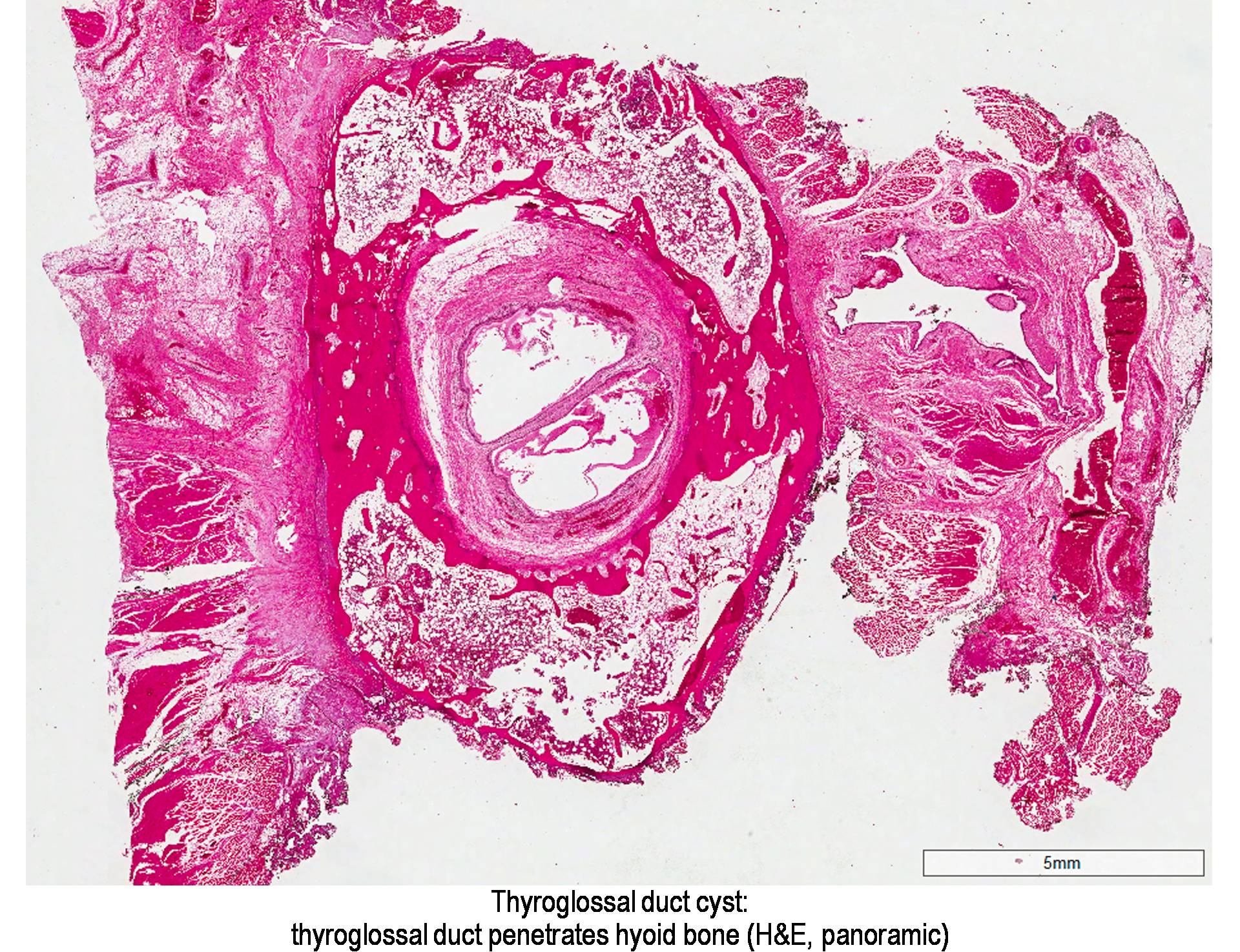
- Most TGD cysts are connected to hyoid bone, which is excised during TGD excision (Sistrunk procedure)
- Prevalence (J Pediatr Surg 1984;19:555, Int J Pediatr Otorhinolaryngol 2003;67:1285):
- 75% thyrohyoid (between hyoid bone and thyroid cartilage)
- 25% suprahyoid, including submental
- 2 - 4% intralingual (base of tongue)
- Rare sites: suprasternal, intrathyroid, mediastinal
- TDG cysts may present lateral to midline in 10-20%, but never lateral to large neck vessels
- Mainly deviate to the left, because levator glandulae thyroideae is ordinarily found to the left (Surg Clin North Am 1953:633)
- Often in the region of thyroid cartilage which moves superficial cyst from the median
- Can be dislocated due to inflammation/fibrosis or previous surgery (Int J Pediatr Otorhinolaryngol 2003;67:1285)
Diagrams / Tables
Pathophysiology / Etiology
- During embryonic development, thyroid gland remains connected to the foramen cecum (floor of primordial pharynx) and hyoid bone by TGD; the duct gradually disappears by the 10th week of development
- If involution fails, TGD remnants may persist anywhere along the pathway of thyroid descent
- The only normal remnant of the duct is the pyramidal lobe of the thyroid gland, which is seen in about 40% of the population (Thyroid 2013;23:84)
- Cystic dilation is a result of secretion from the lining epithelial cells
- Inflammation of lymphoid tissue adjacent to the TGD (repeated respiratory infections) may stimulate the epithelial remnants of thyroglossal tract to undergo cystic changes (BJS 1925;12:561)
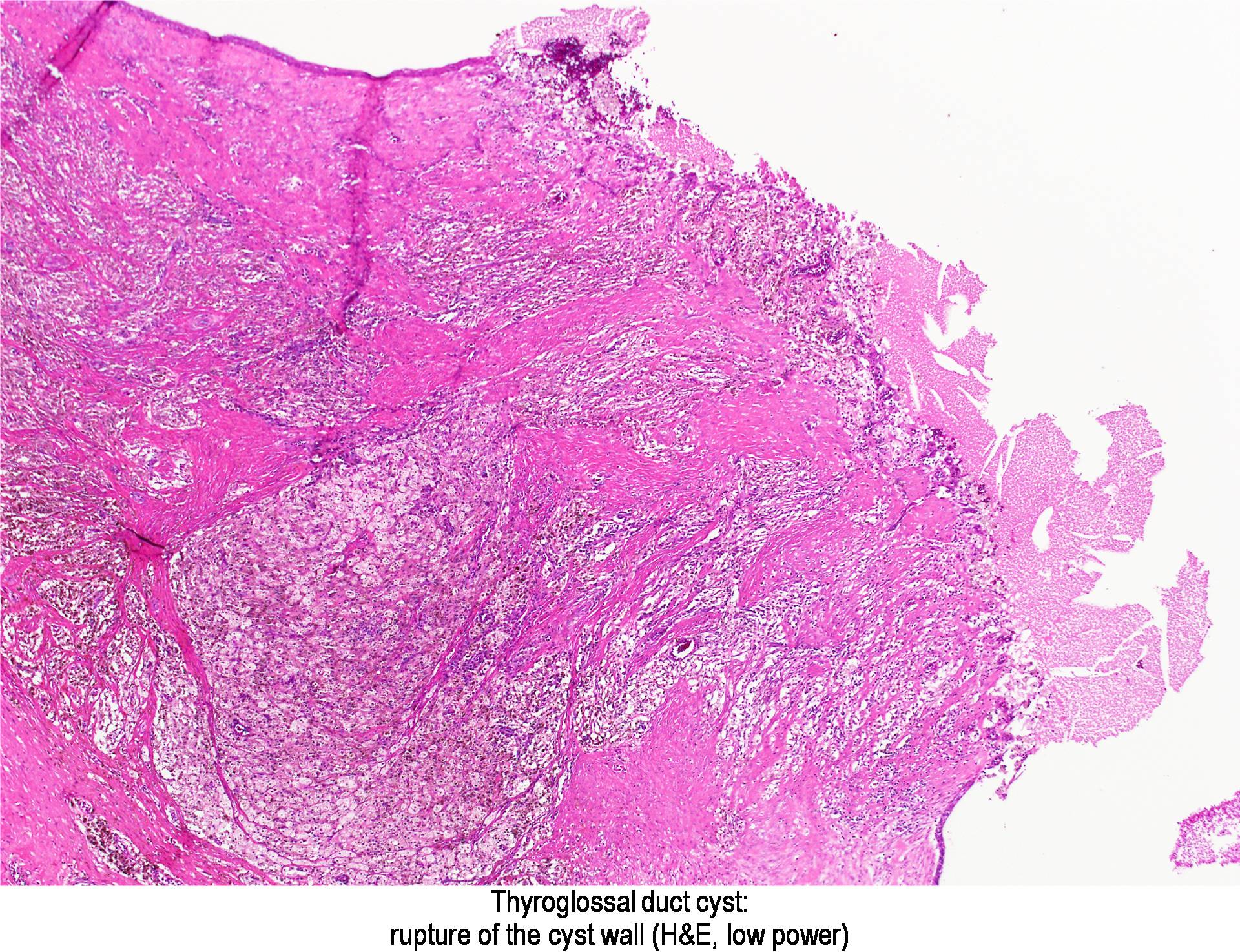
- Sinus is formed secondary to trauma, inadequate surgery drainage or spontaneous rupture of infected TGD cyst, e.g. due to microbial contamination from oral cavity via foramen cecum
Clinical Features
- Most patients are asymptomatic, with a slowly enlarging painless cystic mass in the midline anterior neck (perihyoid), 2 - 4 cm in size (Auris Nasus Larynx 2008;35:11)
- On physical examination, the cyst can be soft or firm and move upward on swallowing or protrusion of tongue
- Infected TGD cyst occurs in 30% of patients, who present with pain, local inflammation, sometimes with draining sinus or fistula (Semin Pediatr Surg 2006;15:70)
- After radiation therapy for unrelated head and neck cancer, TGD may enlarge and undergo cystic transformation (AJNR Am J Neuroradiol 2009;30:800)
- Lingual TGD cyst may cause dysphagia, choking and cough; in neonates, may cause feeding problems, respiratory compromise and even sudden death
- Rarely (<1%), TGD may give rise to tumors, usually papillary thyroid carcinoma, but also benign follicular adenomas, including Hurthle cell adenoma
Diagnosis
- Based on typical clinical manifestations supported by radiological findings and confirmed by postoperative histopathology
- Ultrasound is the preoperative investigation of choice (Radiographics 2014;34:37):
- Echogenic characteristics of TGD cyst are cyst location, relation to the hyoid bone and echotexture of thyroid gland
- CT and MRI play a supplementary role to more accurately delineate anatomy of large cysts, and MRI may be utilized to define a residual fistulous tract in recurrent disease (Auris Nasus Larynx 2008;35:11)
Radiology Description
- Ultrasound (Korean J Radiol 2015;16:419, Clin Radiol 2005;60:141):
- Midline (just under the hyoid bone) well circumscribed anechoic cystic lesion in simple TGD cyst
- Pseudosolid appearance, when the cyst contains a proteinaceous fluid, cholesterol crystals and keratin
- Heterogeneous pattern with internal echoes in cases of previous infection or hemorrhage
- Most pediatric TGD cysts have a pseudosolid appearance
- True solid component suggests risk of TGD malignancy
- CT with contrast shows a well delineated cystic lesion with capsular enhancement (especially in infected cysts), and its relation to hyoid bone (Indian J Surg 2011;73:28)
- MRI demonstrates low signal intensity with T1 weighted sequences and high signal intensity with T2 weighted sequences which do not restrict diffusion; expansion and destruction of the cartilaginous structure of the hyoid (Radiographics 2014;34:37)
- Scintigraphy potentially can detect functioning thyroid tissue in TGD (Thyroid 2007;17:341)
Prognostic Factors
- Excellent prognosis after complete excision, even if carcinoma is present
- Recurrence rate after Sistrunk procedure is less than 5%; however, if the central hyoid bone is not removed, TGD cyst may recur in 25% cases (Surg Gynecol Obstet 1949;89:727)
- Risk factors for complications and recurrence are young age (<10 y.o.), lobulated, infected or ruptured cyst, skin involvement and failure to excise the midportion of the hyoid bone and the suprahyoid tract (Am J Surg 1986;152:602)
Case Reports
- Various locations
- Newborn with TGD cyst on the tongue base (Case Rep Obstet Gynecol 2016;2016:781630)
- Infant with lingual TGD cyst (Respir Care 2014;59:e98)
- 10 year old girl with intrahyoid TGD cyst (Indian J Otolaryngol Head Neck Surg 2007;59:366)
- 28 year old man with migratory TGD cyst (Indian J Radiol Imaging 2010;20:115)
- 31 year old man with intralaryngeal TGD cyst (Pan Afr Med J 2015;22:294)
- 40 year old woman with TGD cyst within the mediastinum (J Thorac Cardiovasc Surg 2007;133:1671)
- 45 year old woman with intrathyroid TGD cyst (Int J Clin Exp Pathol 2015;8:7229)
- Complications
- Infant died of fatal asphyxia by a TGD cyst (Am J Forensic Med Pathol. 2008;29:251)
- 6 year old girl with hypothyroidism after excision of TGD cyst (J Pediatr 2013;162:427)
- 14 year old girl with infected TGD cyst (Case Rep Dent 2011;2011:978263)
- 18 year old man with follicular adenoma in TGD (Braz J Otorhinolaryngol 2007;73:430)
- 18 year old woman with Hurthle cell adenoma arising in a TGD cyst (Head Neck 1993;15:348)
- 23 year old woman with infected TGD cyst (West J Emerg Med 2009;10:205)
- 28 year old man with follicular adenoma in TGD cyst and papillary carcinoma in the thyroid (Am J Otolaryngol 2005;26:348)
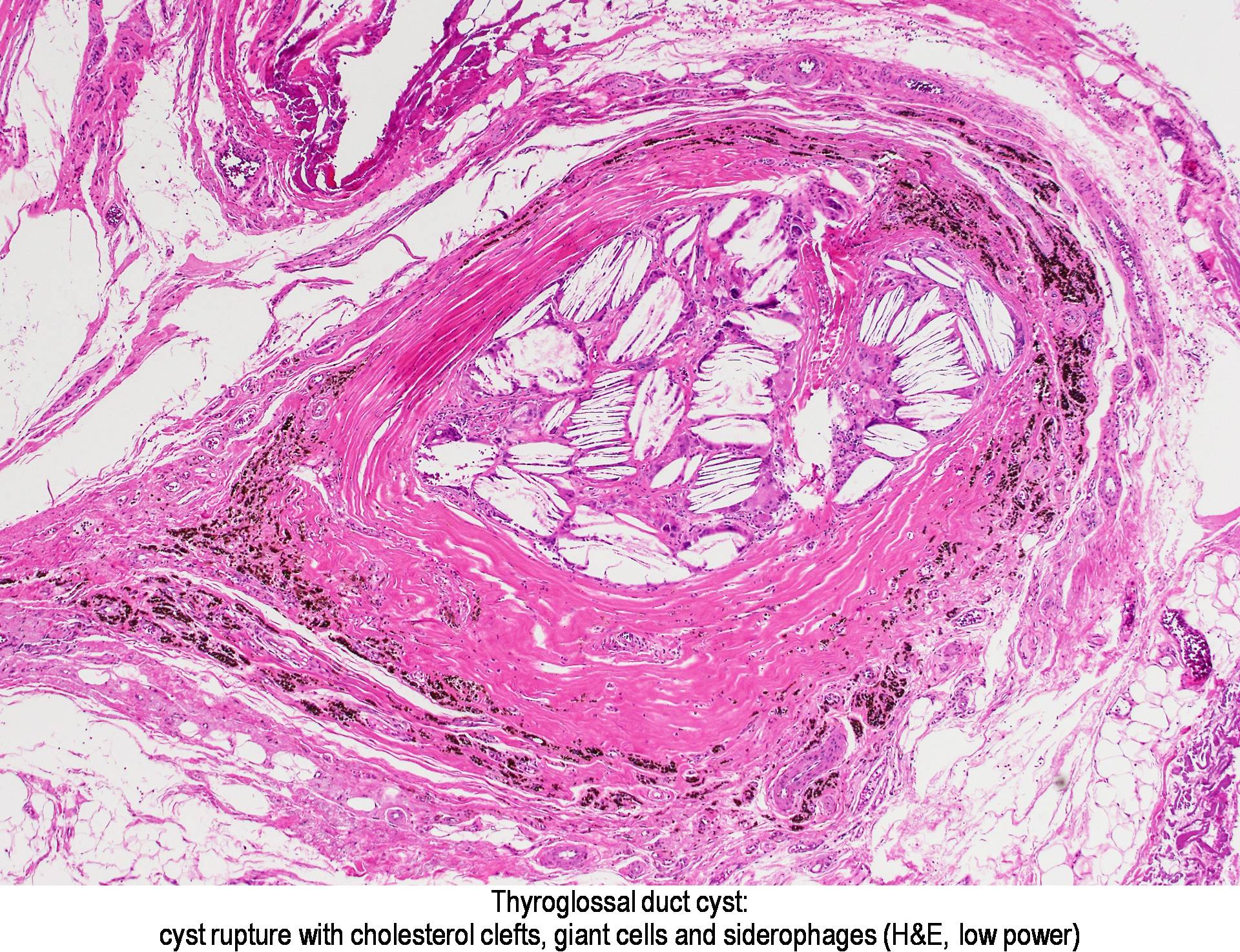
- 40 year old male with ruptured TGD cyst leading to xanthogranulomatous inflammation (Head Neck Pathol 2015;9:530)
- 46 year old female with extravasation mucocele arising from a lingual TGD remnant (Case Rep Otolaryngol 2015;2015:326251)
- 55 year old man died of fatal asphyxia by a TGD cyst (J Clin Forensic Med 2006;13:349)
- 65 year old man with giant TGD cyst (Indian J Otolaryngol Head Neck Surg 2011;63:27)
- Unusual combinations
- 7 year old boy with double cyst originated from a single TGD (J Pediatr Surg 2008;43:748)
- 15 year old girl with cartilage within a TGD anomaly (Int J Pediatr Otorhinolaryngol 1988;15:205)
- 18 year old woman with epidermal, TGD and lymphoepithelial neck cysts (J Oral Maxillofac Pathol 2013;17:479)
- 20 year old man with ectopic thyroid in the floor of the mouth and functioning TGD cyst without orthotopic thyroid gland (Singapore Med J 2013;54:e149)
- 35 year old woman with metachronous TGD cyst and inferior parathyroid cyst (Kaohsiung J Med Sci 2008;24:487)
- 52 year old woman with ectopic thyroid nodule in TGD (Korean J Intern Med 2011;26:218)
- 85 year old woman with large TGD cyst and lingual hemangioma (BMJ Case Rep 2011;2011)
Treatment
- Surgery is routinely recommended for all patients with TGD cysts
- The treatment of TGD remnants, whether cyst or sinus / fistula, is a complete surgical excision using the Sistrunk procedure
- This consists of a block excision of the entire TGD to the foramen cecum, and removal of the middle third of the hyoid bone (Operative Techniques in Otolaryngology 2004;15:220)
- Incision / draining or sclerotherapy is strictly discouraged
Clinical Images
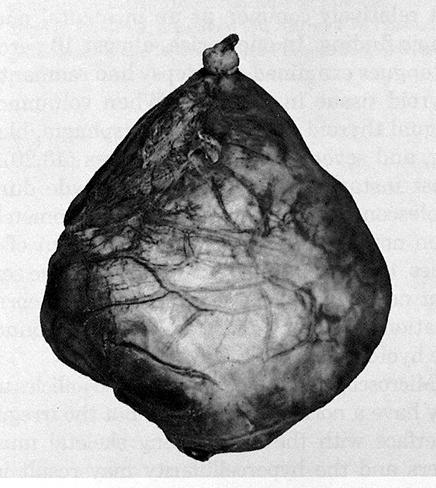
Gross Description
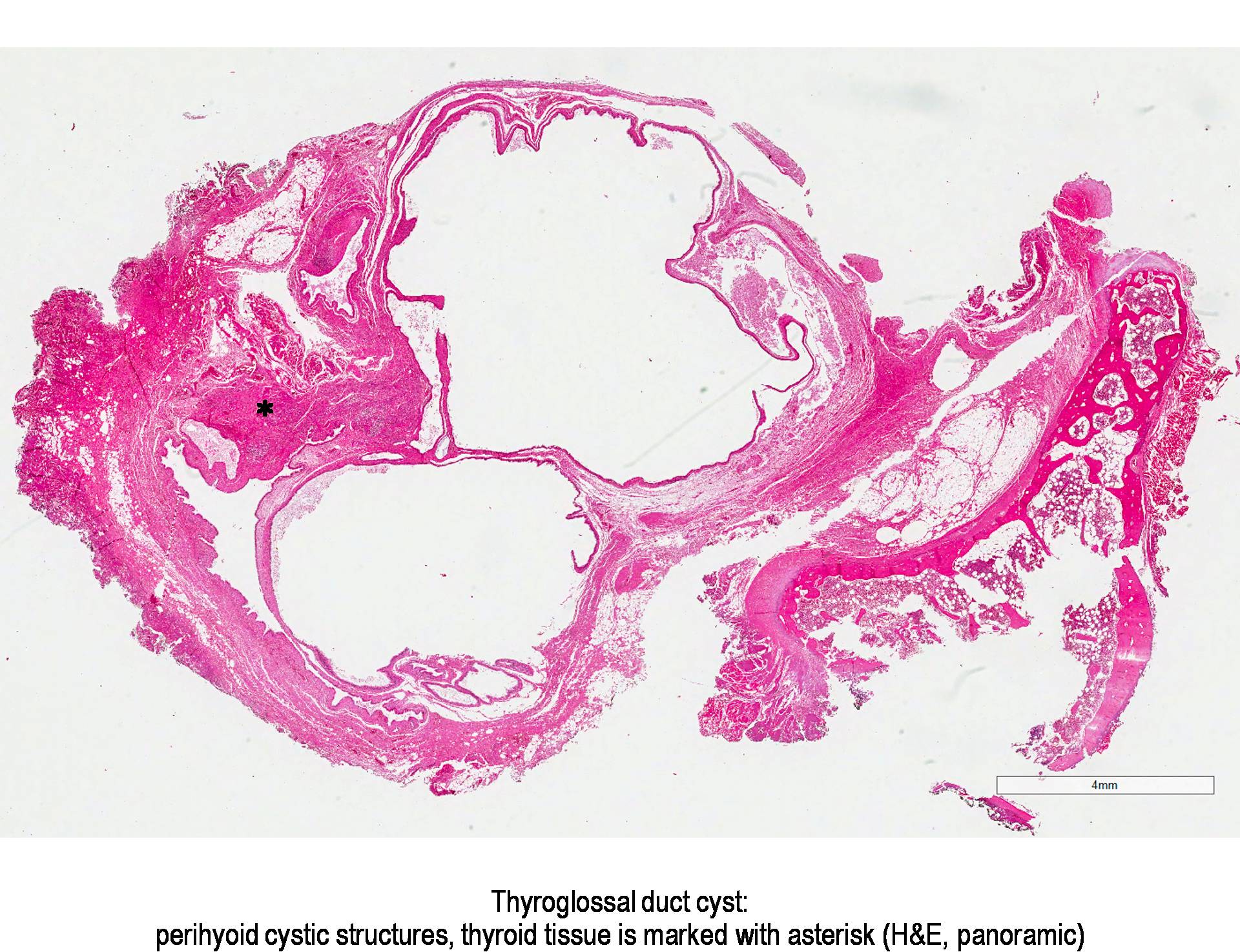
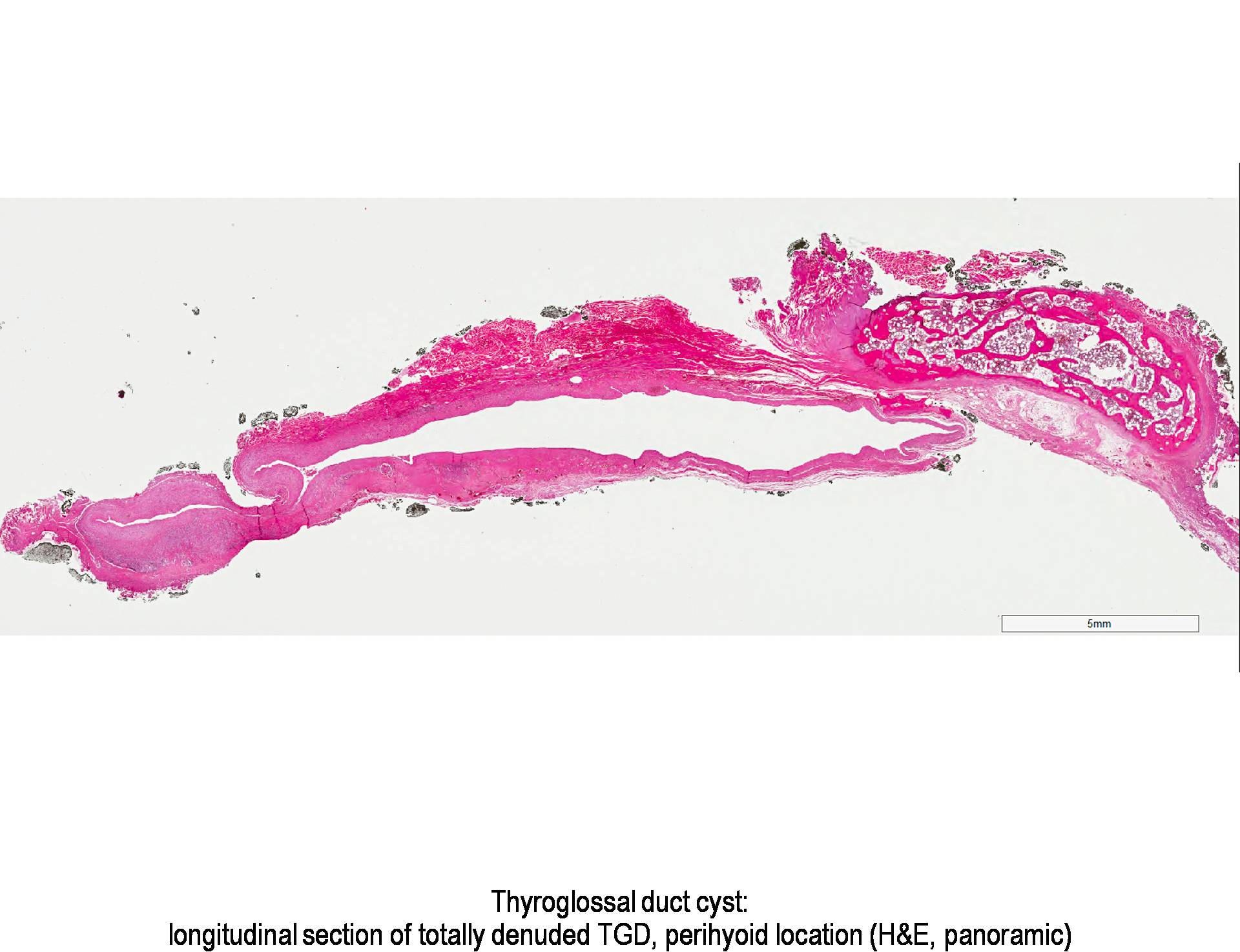
- The thyroglossal duct is a continuous tract from the base of tongue, but occasionally is multiple and aborizing, with a dominant cyst and smaller cysts that are identified microscopically (J Pediatr Surg 1984;19:506, J Pediatr Surg 1991;26:766)
- Cysts are unilocular or multilocular with rounded, smooth external surfaces
- Cyst has a mean diameter of 2 cm, range 0.2 - 7 cm (J Am Coll Surg 2002;194:274, Endocr Pathol 2015;26:75), giant cysts >10 cm are also described (Ann Surg 1954;139:123)
- Cystic content includes clear mucinous or viscous fluid / gel having a broad range of color (clear, yellow-tan, red-brown and gray-white) and degree of opacity; infected cysts contain purulent exudate
Gross Images
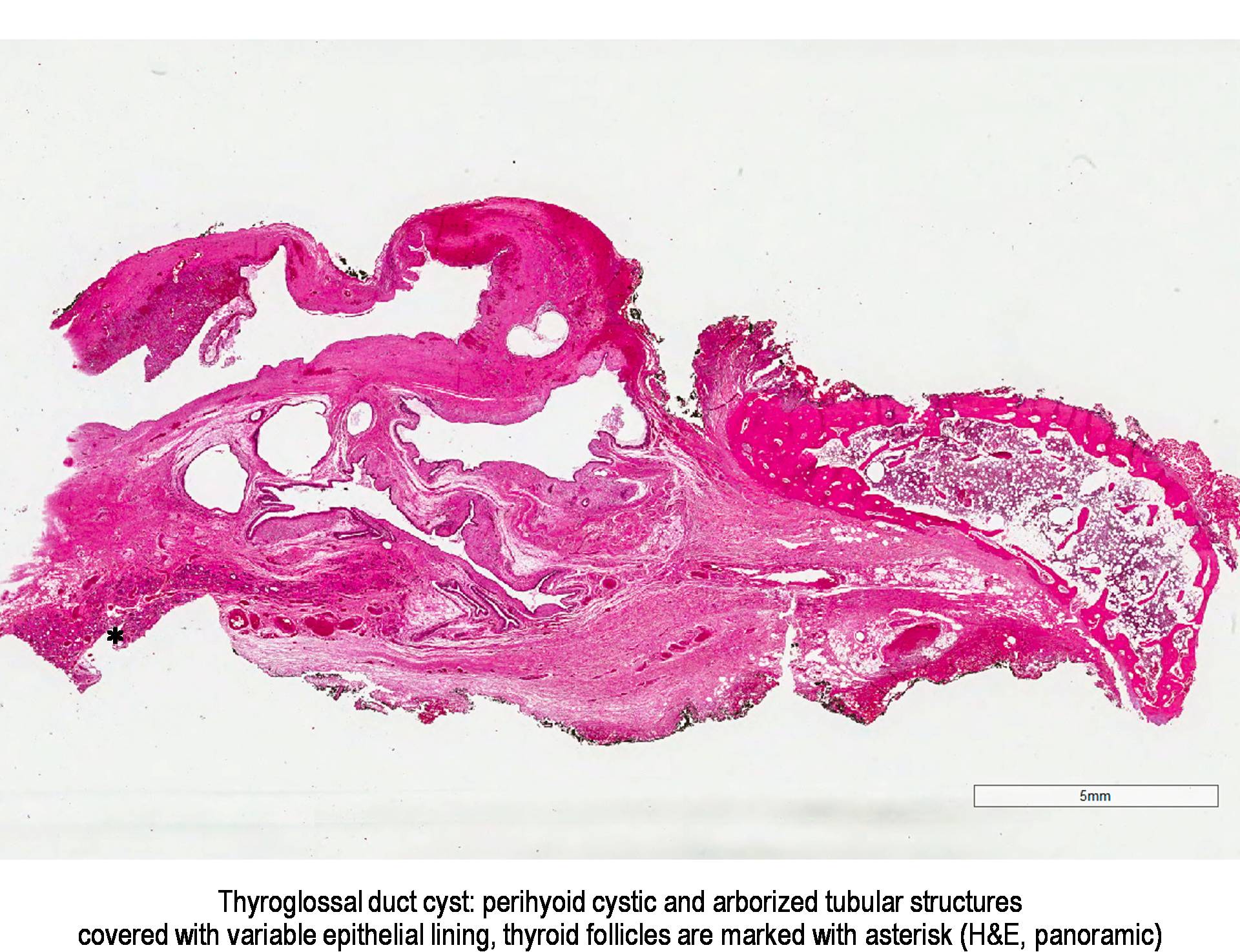
Micro Description
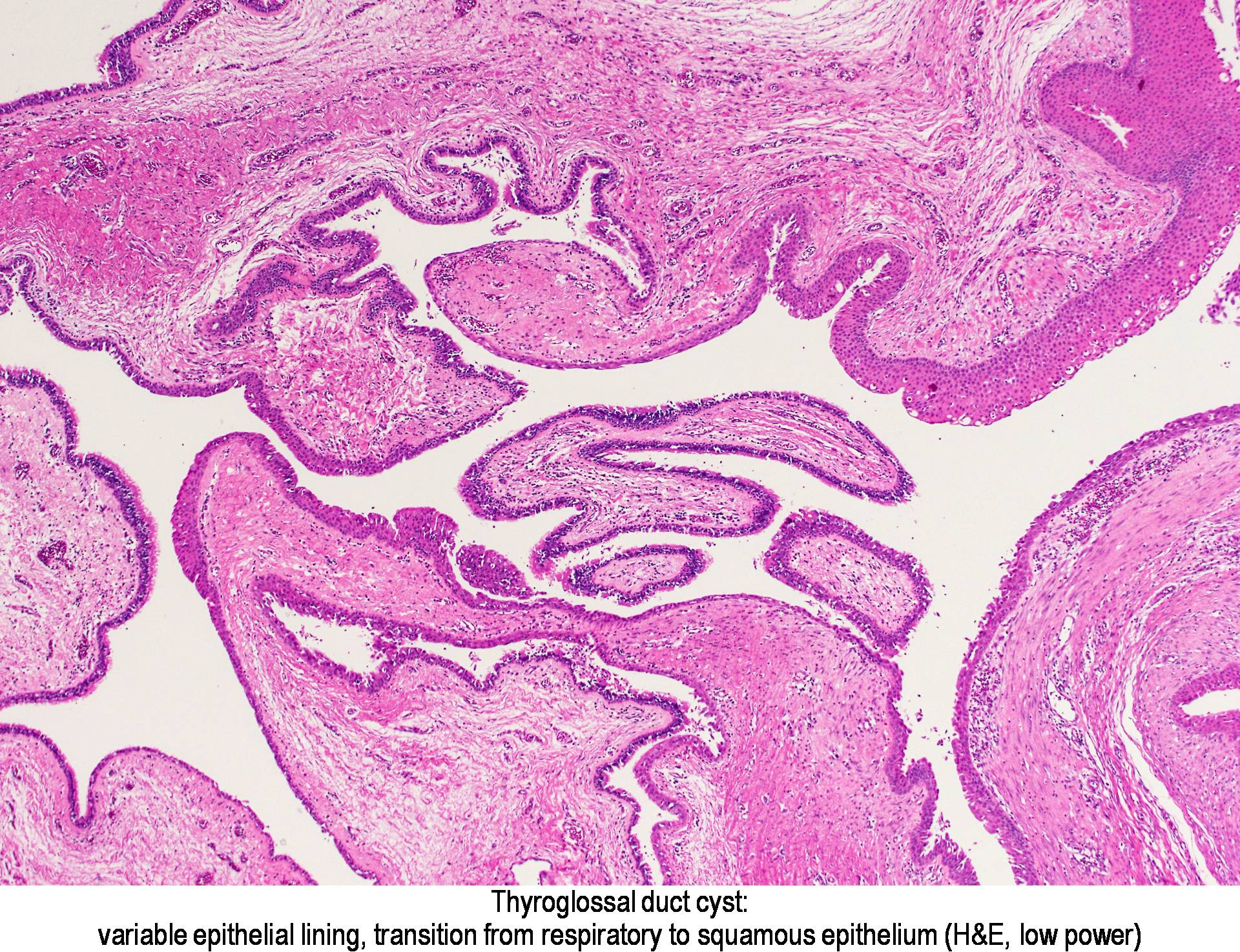
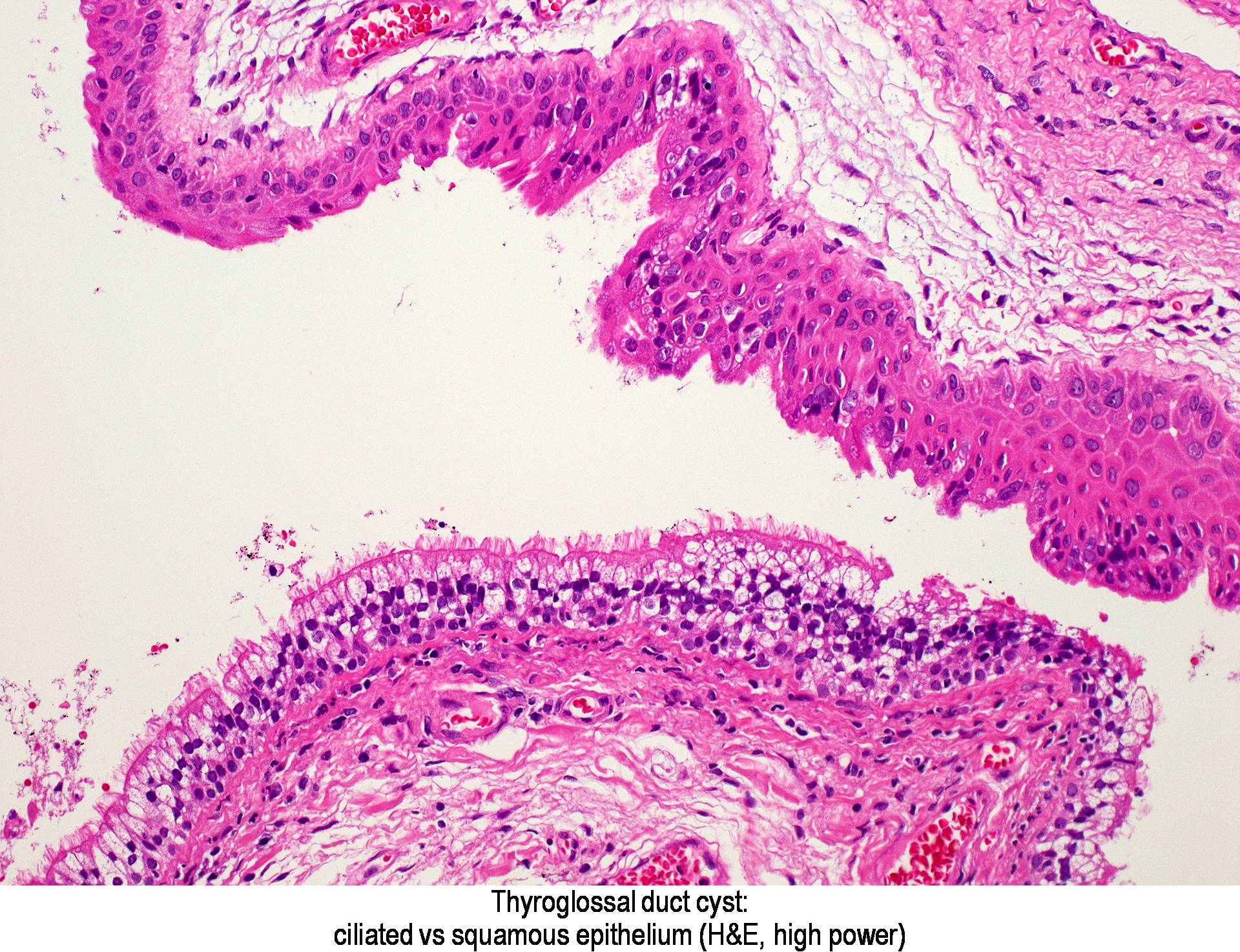
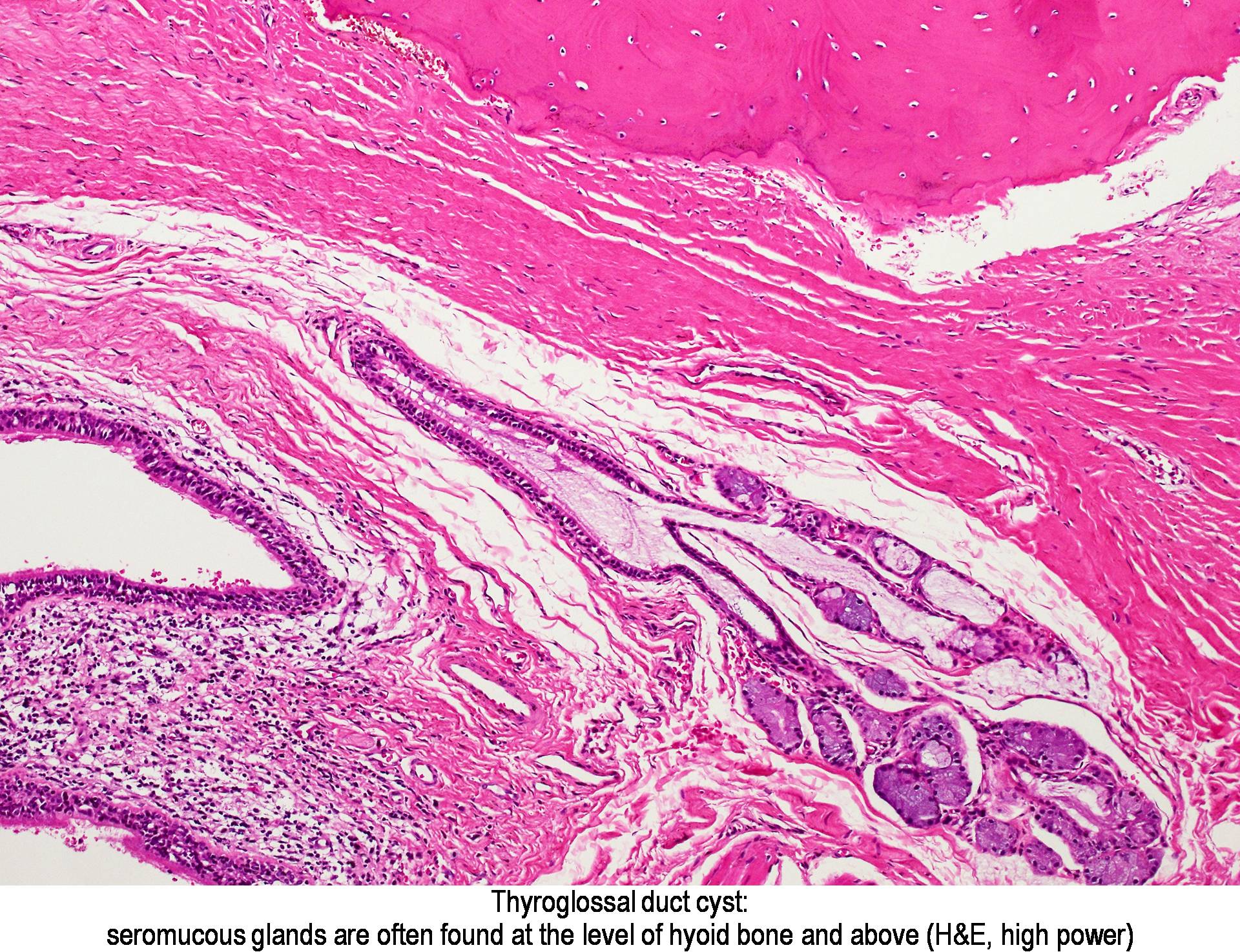
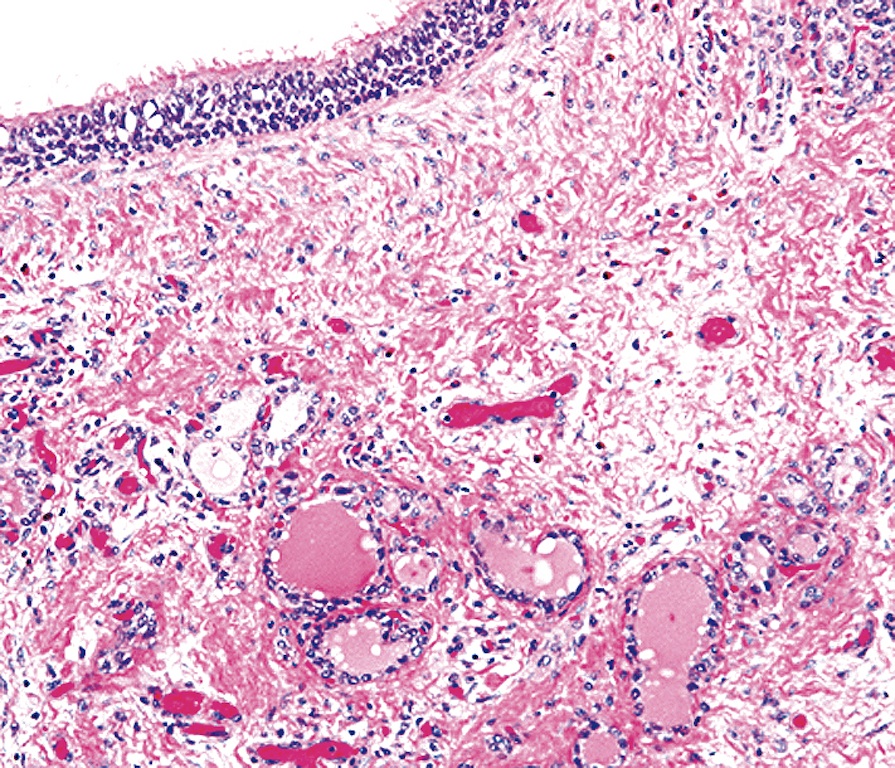
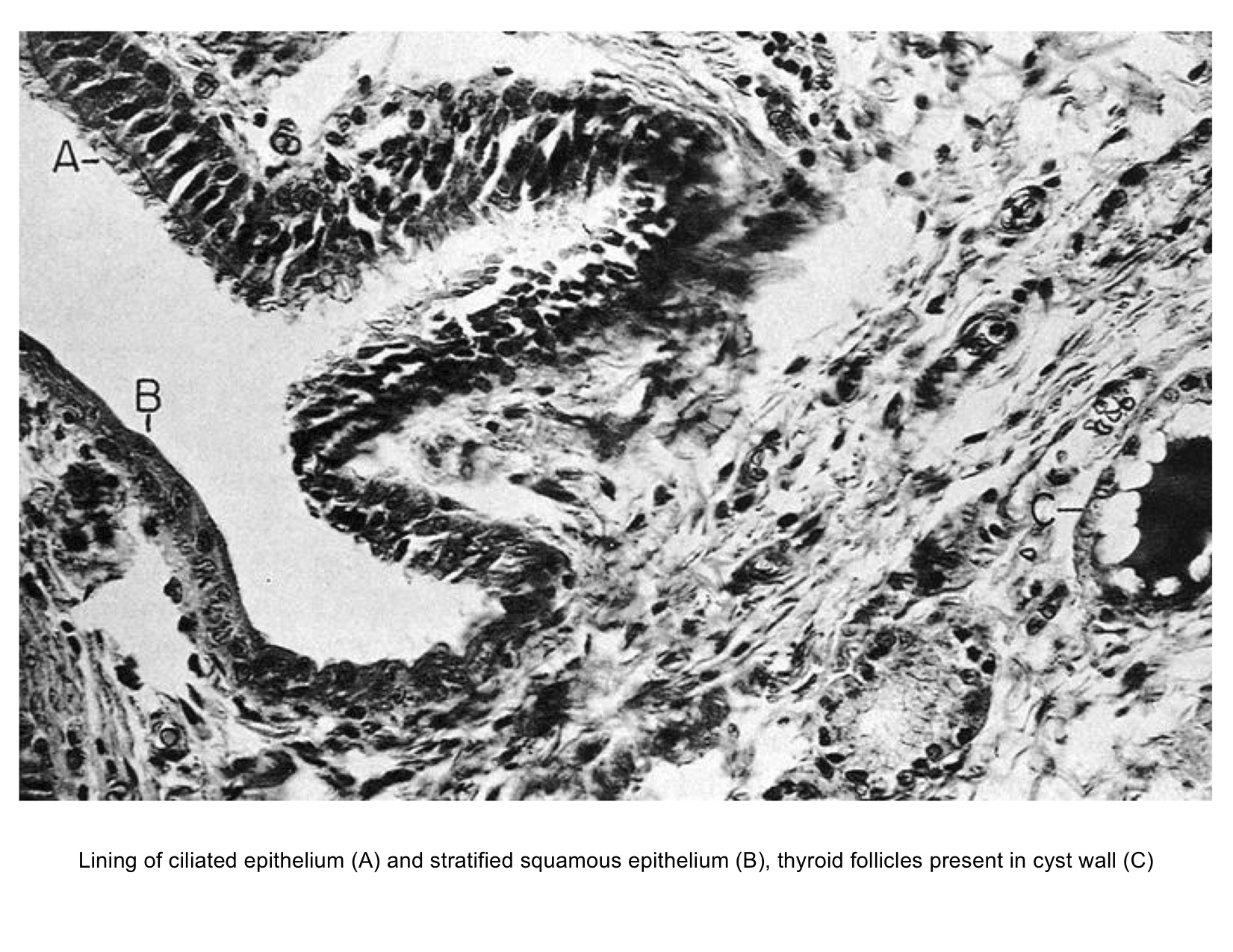
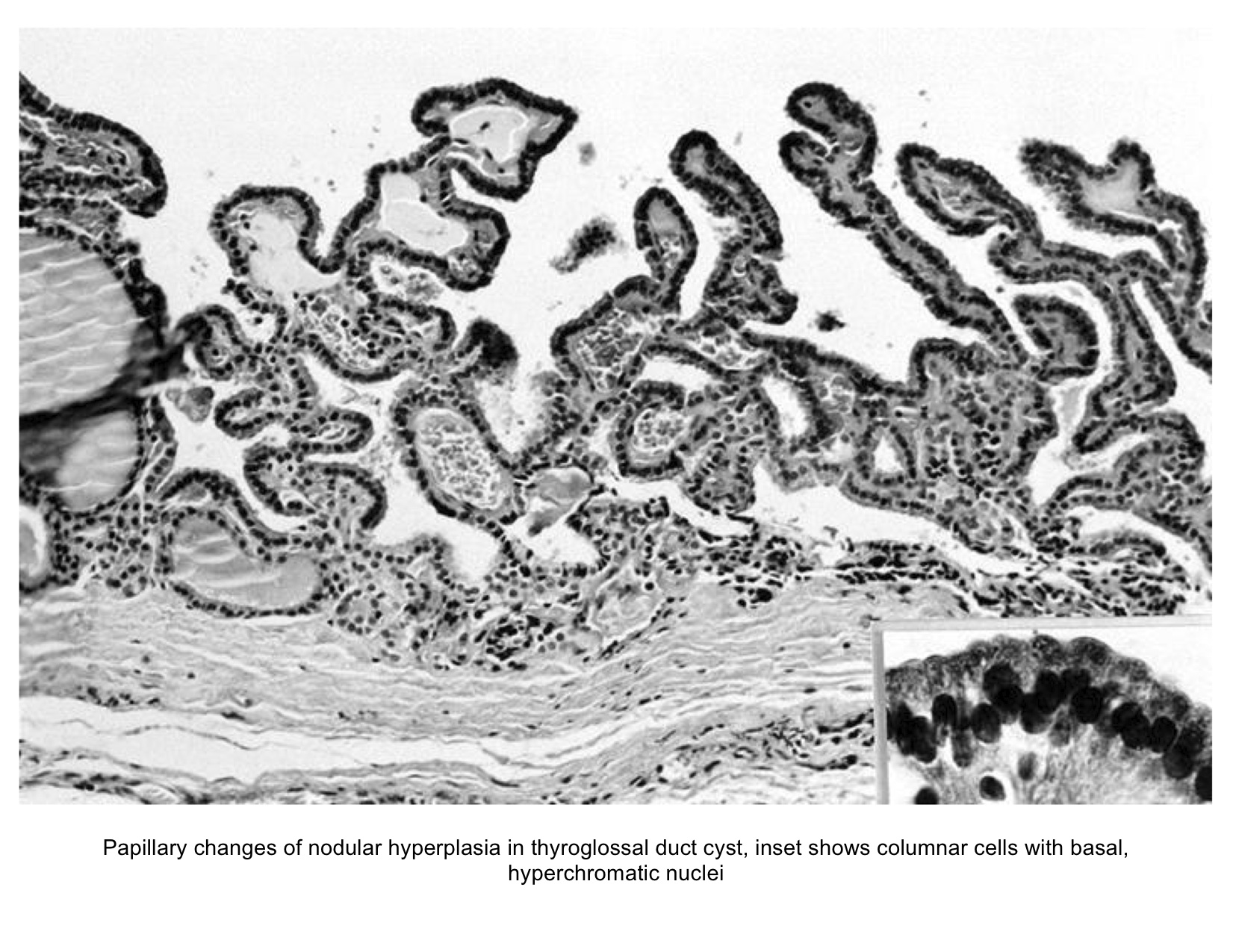
- Type of epithelial lining varies by site, and combinations of the types below can be seen in a single cyst (Head Neck Pathol 2013;7:50):
- Ciliated pseudostratified columnar (respiratory) epithelium in lower neck, perhaps due to its close proximity to upper respiratory tract
- Non-keratinizing squamous epithelium in higher neck (near tongue and foramen cecum), also can be of metaplastic origin in inflammatory settings
- Stratified cuboidal epithelium at level of hyoid bone
- Very often the cyst is denuded of epithelium, at least focally, which reflects epithelial damage by inflammation
- Secondary inflammation is common, especially in sinus tract (J Pediatr Surg 1984;19:506):
- Intense lymphocytic infiltration, rarely arranged into lymphoid follicles
- Admixture of neutrophils (if the cyst is infected)
- Granulation tissue and fibrosis
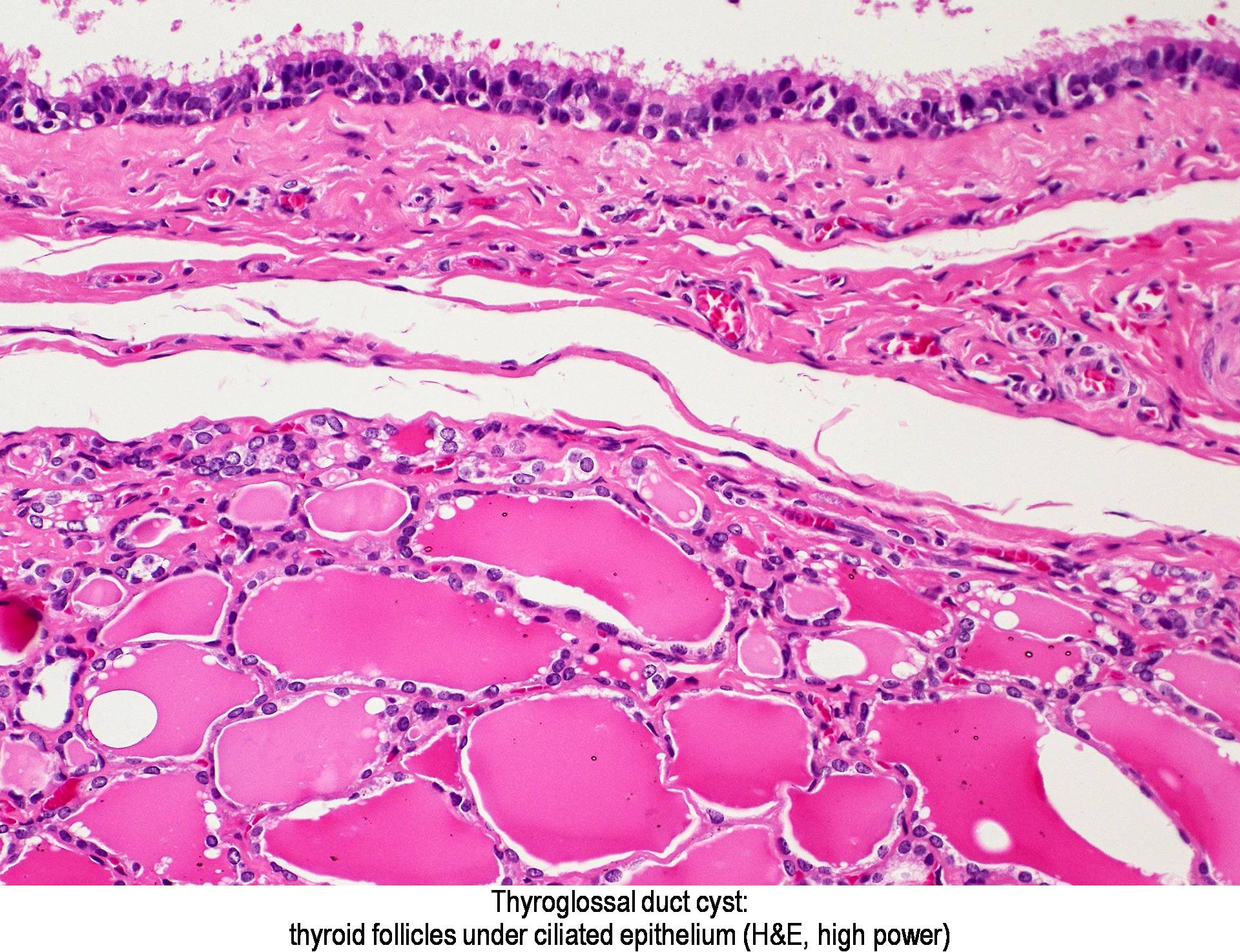
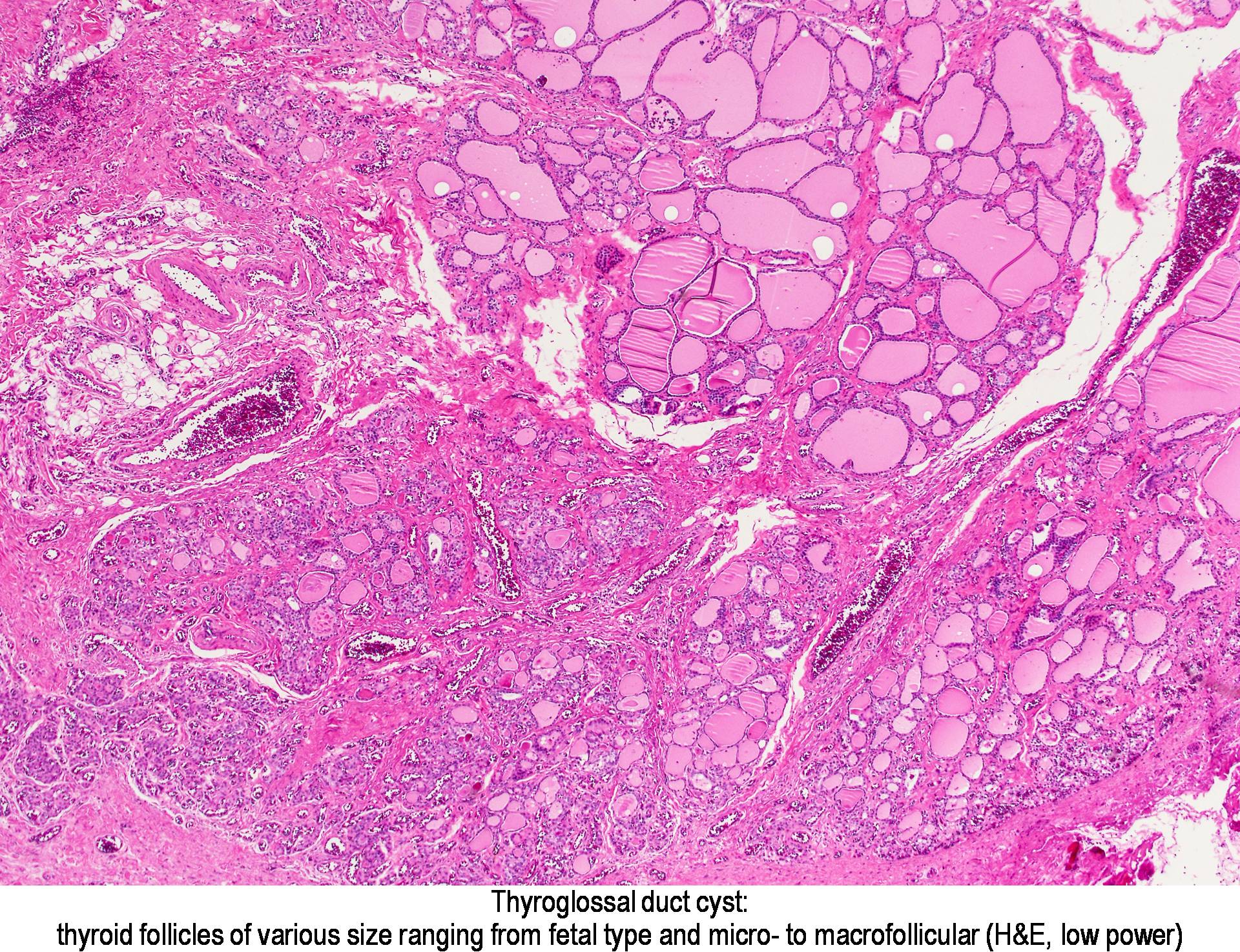
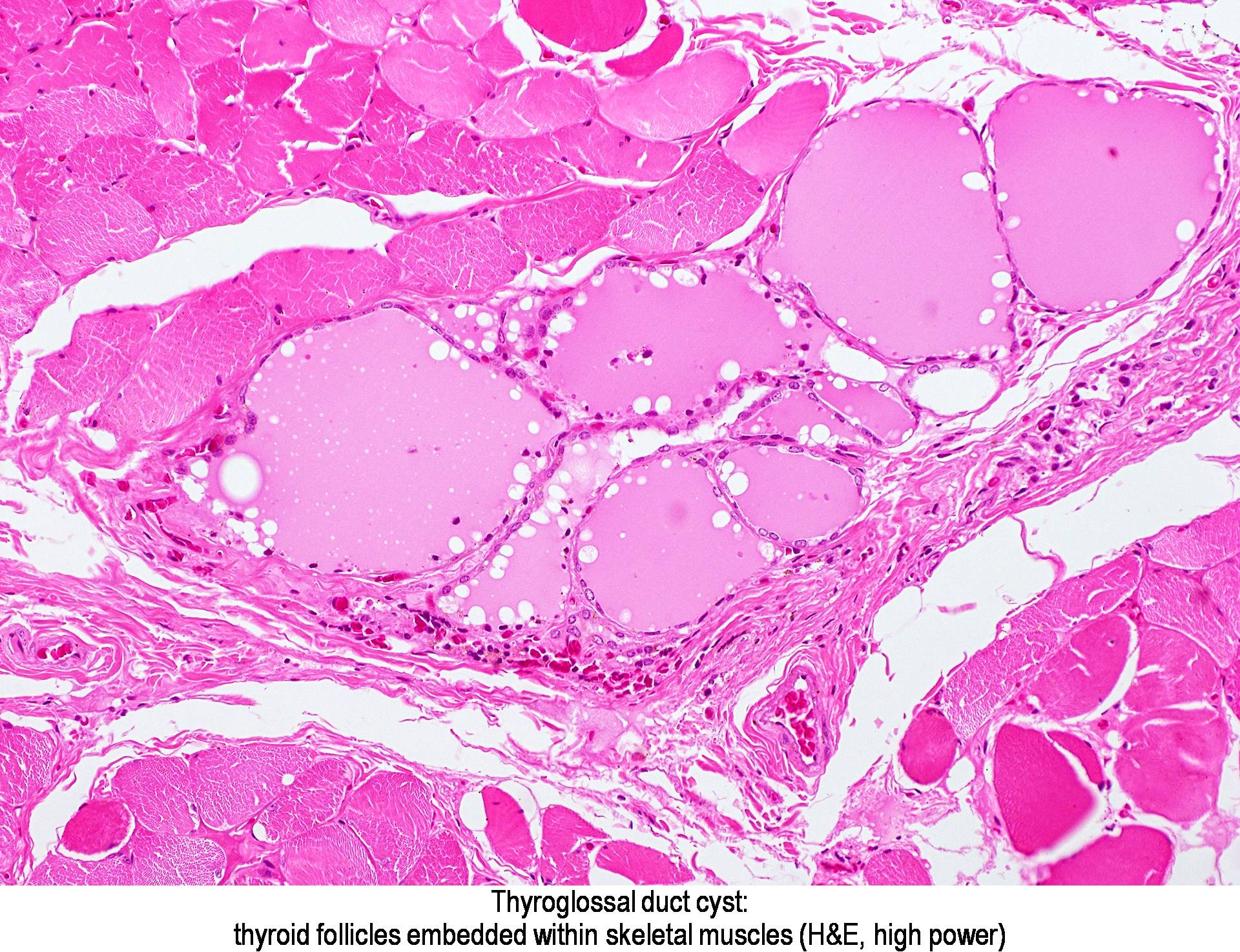
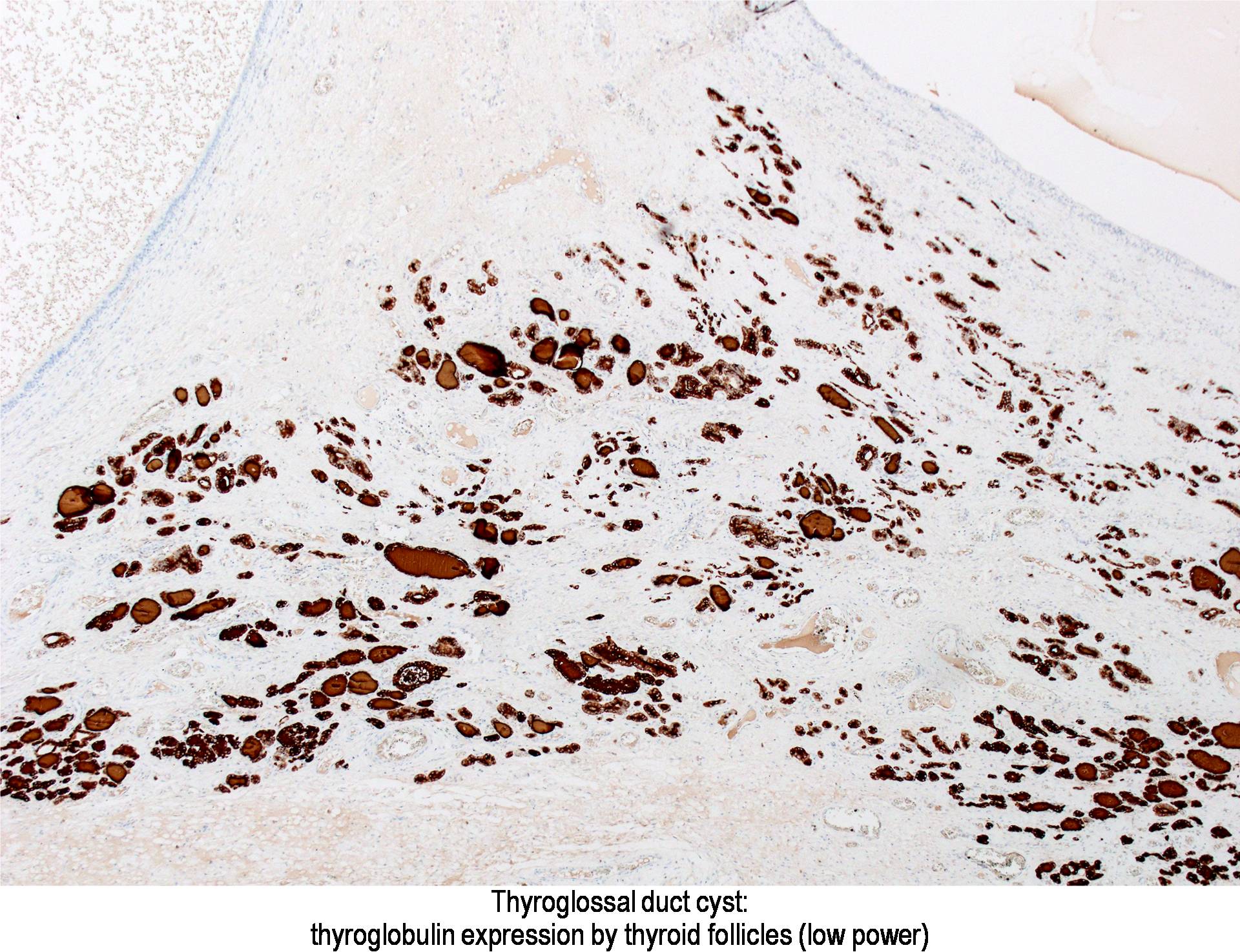
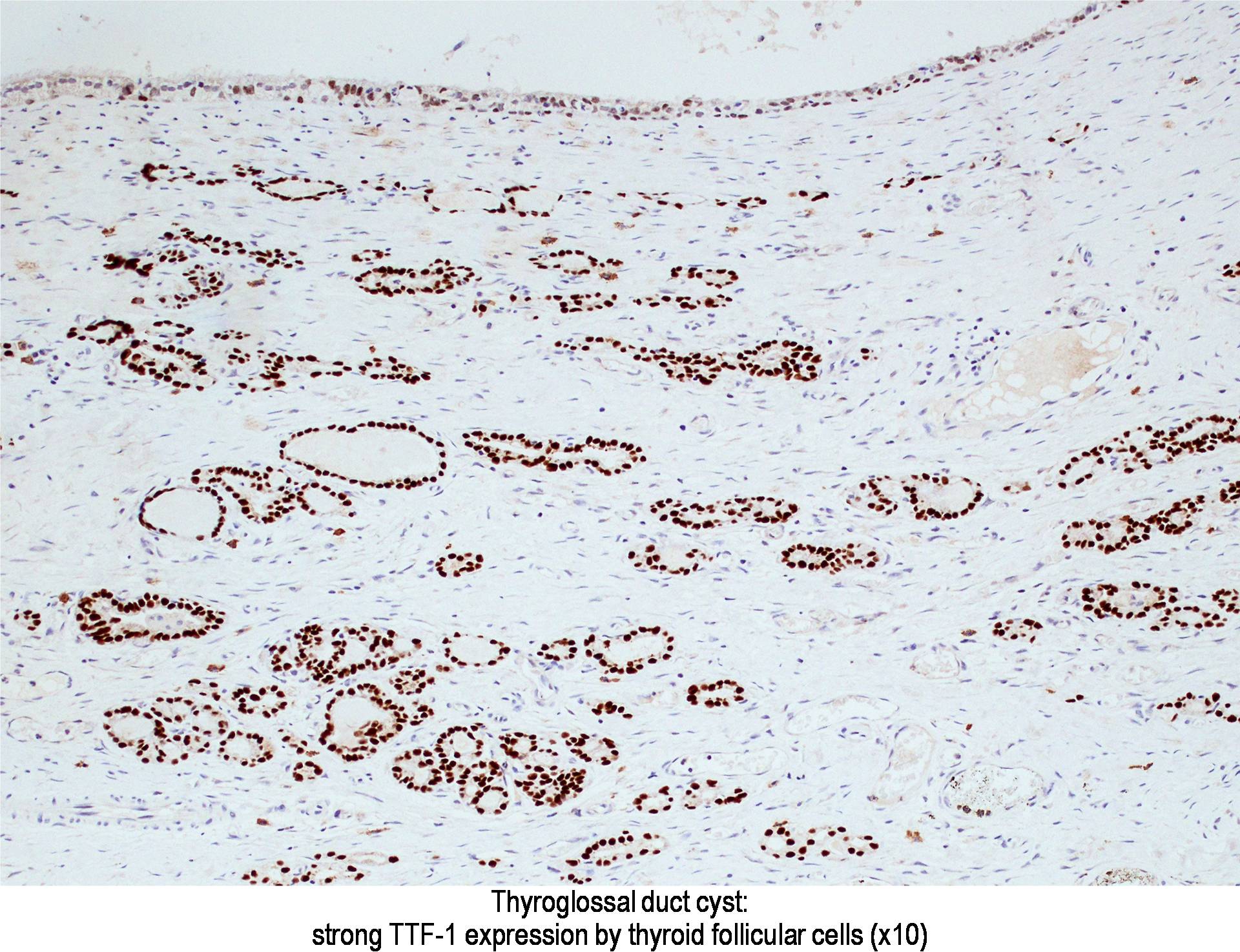
- Thyroid follicles in the cyst/duct wall:
- Found in 30-60%, with higher yield on serial sections
- More common in infra- vs. suprahyoid remnants, on the right paramedian side (Ann Otol Rhinol Laryngol 2000;109:1135)
- Seen in small irregular groups
- Thyroid epithelium may be normal or rarely hyperplastic or neoplastic
- Thyroid tissue often hidden by inflammation (Laryngoscope 2001;111:1002)
- Absence of thyroid tissue does not exclude the diagnosis of TGD cyst
- Mucous salivary-type glands can be found in the cyst wall, frequently in lingual and suprahyoid locations (Ann Otol Rhinol Laryngol 1996;105:996)
- Skin adnexal structures (J Laryngol Otol 2004;118:996)
- Gastric mucosa (Gnepp: Diagnostic Surgical Pathology of the Head and Neck, 2nd Edition, 2009)
- Cartilage (Int J Pediatr Otorhinolaryngol 1988;15:205)
- Bone (J Laryngol Otol 1994;108:168)
- Cholesterol granuloma (Eur Arch Otorhinolaryngol 2009;266:1775)
Micro Images
Images hosted on PathOut server:
Courtesy of Dr. Andrey Bychkov:
Courtesy of Dr. Mark R. Wick:
Images hosted on Other servers:
Courtesy of Dr. Andrey Bychkov:
Courtesy of Dr. Mark R. Wick:
Images hosted on Other servers:
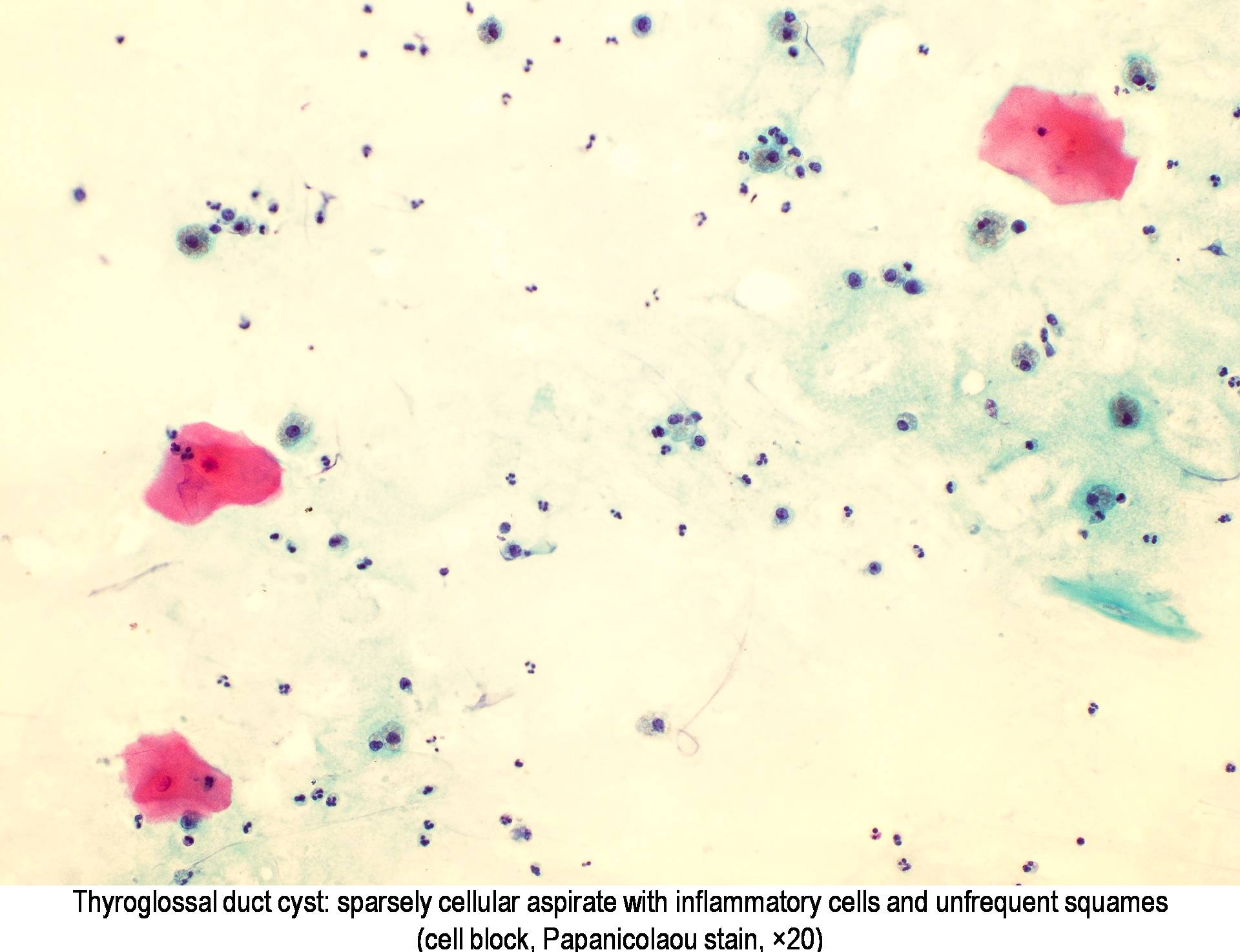
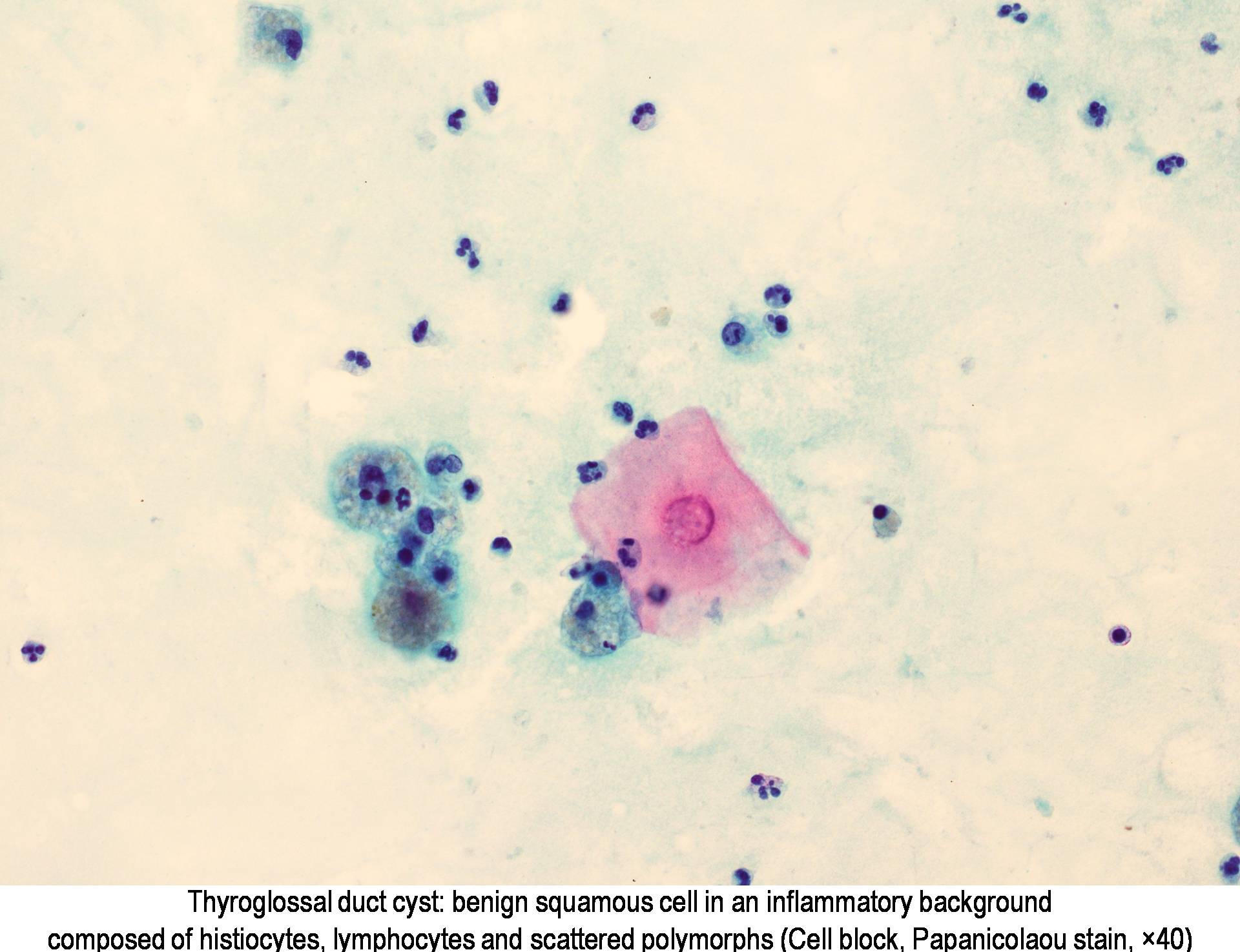
Cytology Description
- Preoperative FNA is moderately sensitive but with many false negatives (Diagn Cytopathol 2005;33:365)
- FNA smears are of low cellularity, with predominant inflammatory cells outnumbering epithelial cells, similar to branchial cleft cyst:
- Macrophages, either foamy or hemosiderin laden
- Mature lymphocytes and neutrophils (predominantly if the cyst is infected)
- Squamous or ciliated columnar epithelium
- Colloid is common, ranging from thick and fragmented to thin and watery
- Admixture of cholesterol crystals
- Thyroid tissue found in <10% of aspirates, likely due to deep embedding in the cyst wall
Cytology Images
Negative Stains
- Thyroglobulin negative epithelial lining, either respiratory or squamous (Virchows Arch 2005;447:9)
- Calcitonin, since C cells are absent in median anlage derivatives (Mills: Histology for Pathologists, 4th Edition, 2012)
Videos
Differential Diagnosis
- Cystic lesions
- Dermoid cyst: filled with sebaceous material, lined by keratinizing epithelium, and having skin appendages in the wall, none of these is observed in TGD (J Pediatr Surg 1984;19:506), in addition, rarely inflamed; aspirate enriched with anucleated squames
- Epidermoid cyst / epidermal inclusion cyst: similar to dermoid cyst, but without skin adnexa
- Branchial cleft cyst: lateral location, lymphoid follicles in the wall; aspirate is more cellular with abundant squamous epithelium
- Lymph node metastasis of papillary thyroid carcinoma with cystic degeneration
- Rare developmental cysts: lymphangioma, lymphoepithelial cyst, thymic cyst (suprasternal), bronchogenic cyst, midline cervical cleft, teratoma
- Rare non-developmental cysts: ranula (upper neck), laryngocele, cystic degeneration of a colloid nodule
- Solid lesions
- Lingual thyroid: resolved by clinical and radiological modalities, orthotopic thyroid is often absent
- Pyramidal lobe of thyroid gland
- Lymph node with reactive hyperplasia
- Lipoma
- Squamous cell carcinoma: atypical cells
- Rare intrathyroidal TGD cysts can be confused with primary thyroid carcinoma
- Histopathological diagnosis of TGD requires optimally evidence of respiratory/squamous epithelial lining and thyroid follicles, which sometimes can be difficult to find due to inflammation and fibrosis; in these situations, a diagnosis of developmental cyst with comment (favor TGD cyst or branchial cleft cyst, etc.) may be an option
http://www.pathologyoutlines.com/topic/thyroidthyroglossal.html


















































































0 nhận xét:
Đăng nhận xét